By Dr David Cork - Osteopath
What is the difference between headaches and migraine?
We have all heard of migraines and headaches but many of us may not know the difference between the two, as a “really bad headache” is often confused with a true migraine.
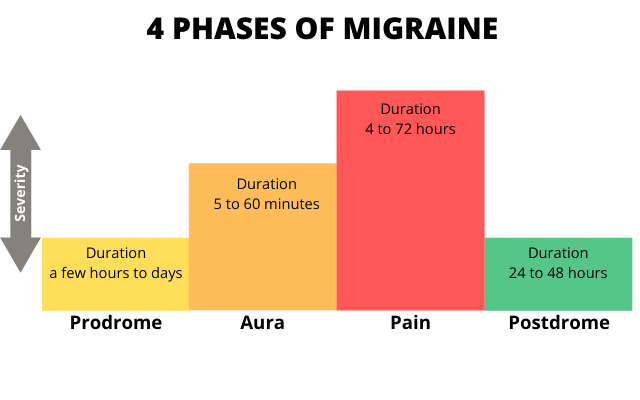
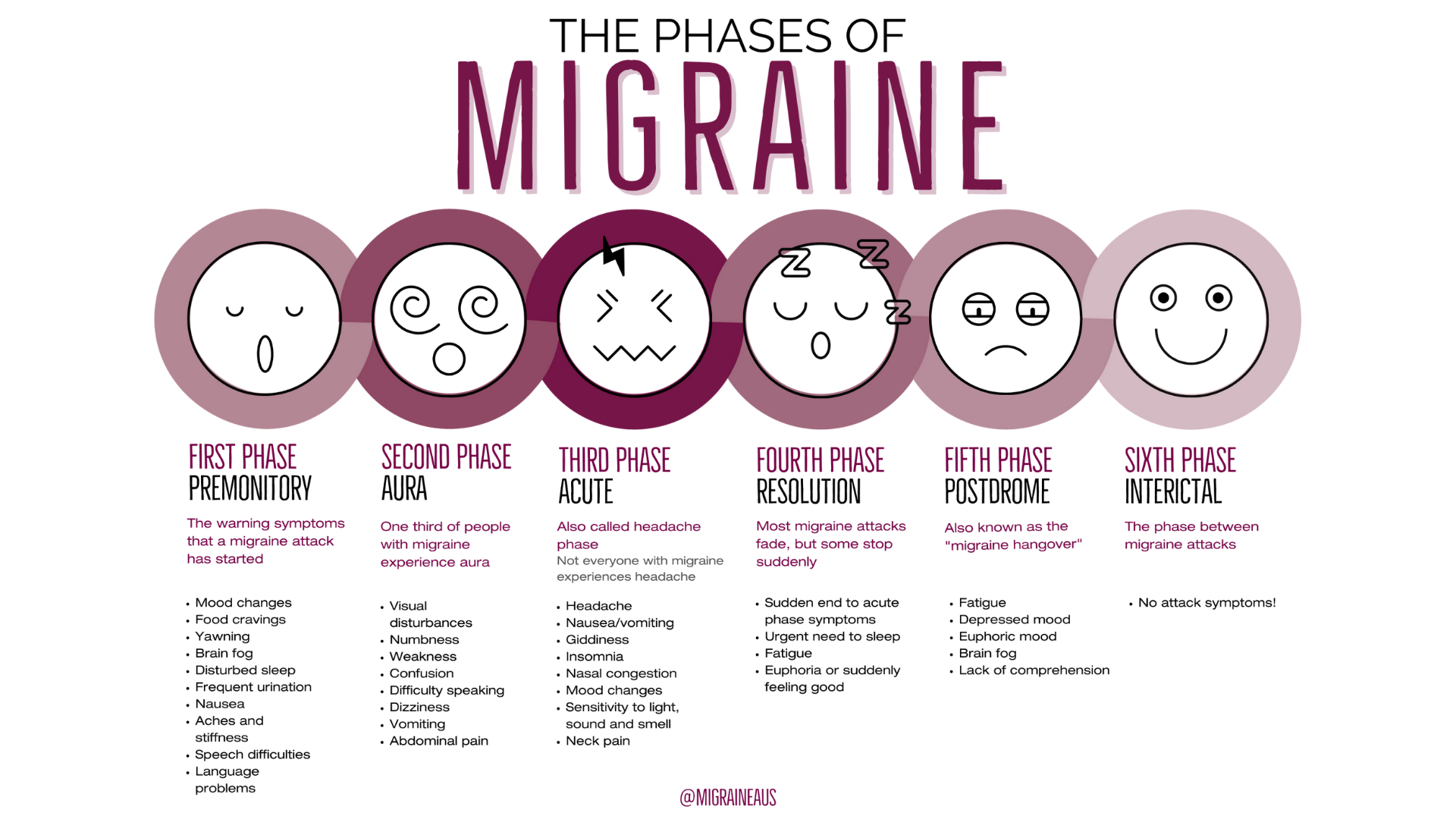
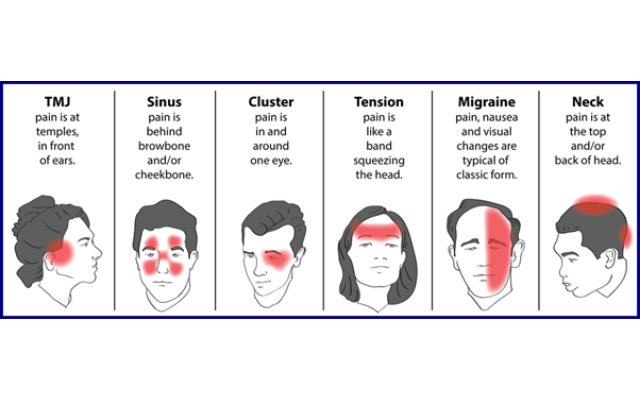
Migraine is often a long term medical condition and people with migraine describe their condition as having ‘attacks’ or ‘episodes’. A Headache (pain felt around the head region) is a common symptom of migraine, although some people with migraine do not experience a headache when they have an episode. Other common symptoms of migraine include nausea, sensitivity to light or sound and visual changes. Migraines often first occur in the peoples early 20s but sometimes in their teens and 30s.
Both headaches and migraine can be intense and debilitating causing significant suffering, impaired quality of life and disability. Many sufferers often worry about when their next headache or migraine may occur causing much stress and anxiety. These conditions can affect employment, the ability to be involved in (and enjoy!) social or leisure activities and if they are significant, may be associated with a deterioration in mental health.