By Dr. David Cork, Osteopath

What is Arthritis?
Arthritis is an umbrella term that covers over 100 different medical conditions primarily relating to the joints, as well as – muscles, ligaments and bones of the body. The most common of these conditions is osteoarthritis. Approximately 1 in 11 Australians have osteoarthritis – that is around 2.2 million people (ABS 2017-2018). The prevalence of osteoarthritis is increasing due high levels of obesity, inactivity and an aging population. It is expected by 2030 that 12% of the population with have osteoarthritis.
Osteoarthritis – How our understanding has changed
Osteoarthritis is a condition that can cause pain, stiffness and restriction in movement and disability.
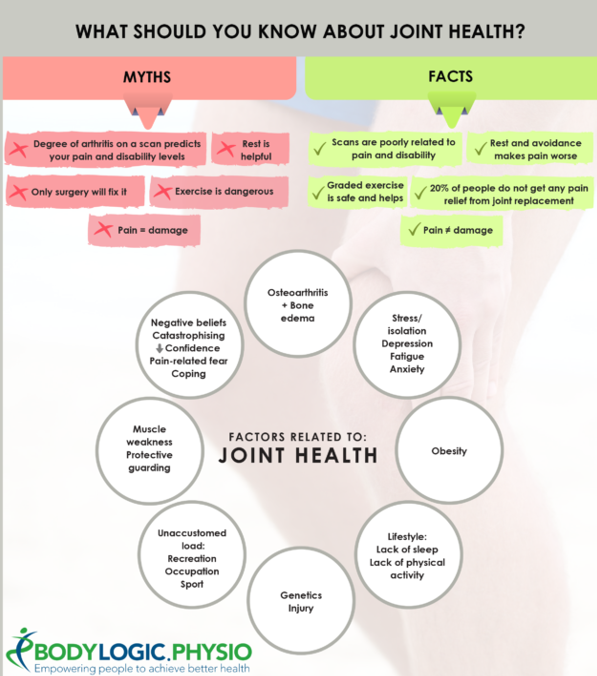
Osteoarthritis used to be seen as “wear and tear” or “degeneration” of joints but we now know this is NOT correct. Joints actually need regular movement and loading to stay healthy. Studies of marathon runners show that they have thicker and healthier cartilage in their knees than the general population. Sedentary individuals also have poorer joint health. Osteoarthritis is now seen to be more related to a poor repairing of joints with a lot of different factors that are thought to lead to systemic inflammation and are poor health in general. Think of osteoarthritis more like “wear and poor repair”
Risk factors of osteoarthritis include:
- Obesity
- Sedentary (lack of physical activity)
- Poor diet and poor general health (diabetes, smoking, cardiovascular disease)
- Previous history of joint trauma e.g. dislocation, ligament rupture or fracture
- Depression, anxiety and other mental health conditions
- Age
- Genetic factors
Osteoarthritis treatment
What treatments are helpful for osteoarthritis?
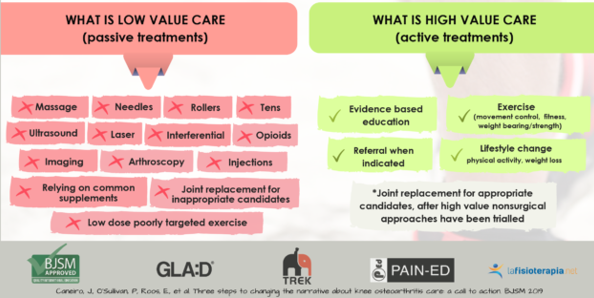
Treatment for osteoarthritis should have 3 main components: physical exercise, education and weight management strategies. These 3 treatments have a multiplicative effect when combined which will lead to significant improvements in pain, ability to do daily activities and significant improvements in overall health.
Exercise
Exercise is an extremely powerful tool in tackling osteoarthritis. Most people incorrectly think exercise is dangerous for joints, but it is in fact the opposite. Cartilage gets healthier with regular exercise and the pain associated with osteoarthritis can actually worsen with rest and avoidance of physical activity.
A study done in Denmark called GLA:D (Good Living with Arthritis: Denmark) showed a supervised exercise program can have a very positive impact on osteoarthritis. After the study’s success it was replicated in the UK, Canada and Australia with now over 30,000 participants. GLA:D has repeated demonstrated that with adequate exercise, patients can have reduced pain, improved function of mobility, increased physical activity level and improved quality of life. When implemented, this exercise program allowed the majority of the participants of this study to avoid surgery and continue to live an active and fulfilling life with osteoarthritis.
What does a good exercise program for osteoarthritis look like?
A good exercise program should be individually tailored to a level that suits the patient regarding the joints affected and the patient’s goals. Typically, an osteoarthritis exercise program will have a range of components; from strengthening exercises (e.g. squats, step-ups, etc.), flexibility (range of motion) exercises, aerobic exercise (e.g. walking, cycling, swimming) and balance/control exercises.
Exercises are monitored and regularly progressed or regressed based on the patients’ needs. Often exercise can be painful or uncomfortable to start with as the body adjusts to the increase in exercise. If you have pain, it is not an indicator of damage to your body. It is safe for you to exercise with pain.
Education
A very important component of a treatment plan to factor in is education. Being educated helps patients manage acute flare-ups of their osteoarthritis, it improves adherence to an exercise program, it helps patients understand their pain and allows patients to learn to skills to modify activities so that they can manage their osteoarthritis by themselves and stay active for the rest of their lives.
Weight Management Strategies
Multiple studies have shown that reducing your weight by 10% can halve pain related to osteoarthritis. Studies also show that high “body fat” negatively impacts joint health via increasing systemic inflammation, meaning it is more than just mechanical loading of the joint.
What treatments are not helpful for Osteoarthritis?
Arthroscopy and corticosteroid injections long-term can both lead to the greater progression of the osteoarthritis as these types of treatment negatively impact cartilage health. Long-term anti-inflammatory medication use has a risk of negative effects on gastrointestinal and cardiovascular systems and are believed to also impact joint health negatively. PRP (Platelet-Rich-Plasma) injections have been shown to be no better than saline (salt water) injections for osteoarthritis. Other factors that can have negative health impacts long term are excessive X-rays and MRIs, also a heavy focus on the results of the imaging can often progress patients down a path that prioritises surgery over trying less aggressive options like an integrative approach implementing allied health services. If you are interested to learn more or start a treatment plan to help with managing arthritis, we have an incredible team of practitioners who can help.