By Jarrod Agosta - Dietitian and Nutritionist
What is PCOS?
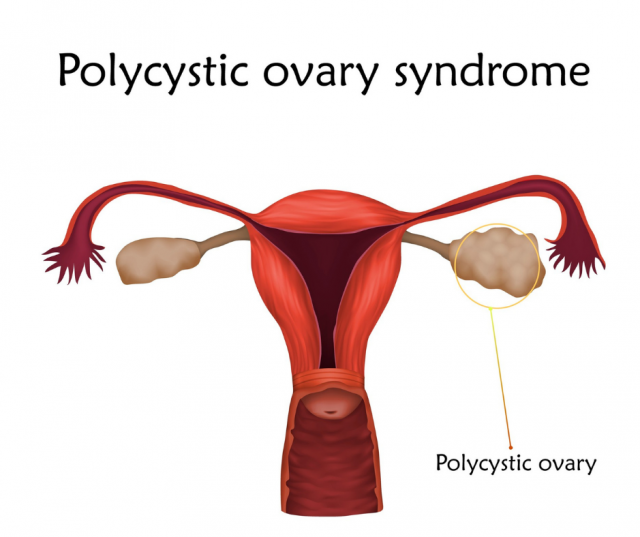
PCOS is a condition that affects the hormones that regulate the menstrual cycle. It is characterised by an abnormal number of follicles (sacs that contain an egg) on the ovaries. The name polycystic -meaning “many cysts”- is a little misleading as, although these follicles look like cysts to the naked eye, in reality they are not cysts (1). In addition to this high number of follicles, the ovaries are also enlarged.
How prevalent is PCOS?
PCOS is the most common endocrine disorder among women of reproductive age and current data suggests that it could affect anywhere from 6-18% of this population (2).
How is PCOS diagnosed?
A syndrome is a group of symptoms. The most commonly accepted diagnosis criteria are that the patient must present with at least two of the following:
- Irregular or absent periods
- Clinical signs or blood test markers of hypoandrogenism (elevated circulating androgen levels such as the hormone testosterone)
- Polycystic ovaries, and the exclusion of other potential causes