By Jarrod Agosta, Accredited Practising Dietitian & Nutritionist
Did you know there are 3 main types of diabetes?
- Gestational diabetes – caused by hormonal changes during pregnancy
- Type 1 Diabetes – an autoimmune condition accounting for around 10% of all diabetes cases
- Type 2 Diabetes – representing 85% of all cases of diabetes
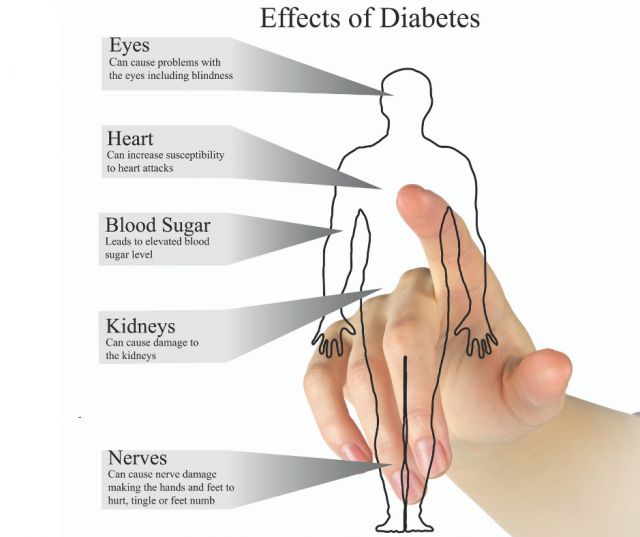
Today we will focus on Type 2 Diabetes (T2DM), a chronic disease that affects approximately 1 million Australian adults (2). But, a further 2 million Australians have pre-diabetes which puts them at high-risk of developing T2DM.
As a Dietitian, I see a lot of clients who present with both pre-diabetes and T2DM who are having a difficult time managing their condition and their blood glucose levels (BGLs). It can be a really stressful situation but the positive news is that diet and lifestyle changes can have a big influence on how both these conditions are managed. This is the area that I work closely with my clients and I’ll go into more detail later in this article, but for now let’s find out a bit more about T2DM.

Evidence shows type 2 diabetes can be prevented or delayed in up to 58% of cases by following a healthy eating plan, maintaining a healthy weight and being physically active (1).